

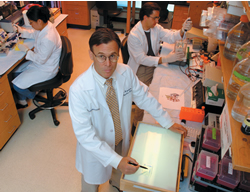
Gastroenterologist Curt Hagedorn (foreground) and researchers Yuri Choi and John LaVoy study why some people respond to HCV therapy and others don't.

Antiviral therapy for the most common form of hepatitis C is expensive, effective only half the time, and often produces severe side effects.

More about hepatitis C
Scientists at a recent NIH conference calculated that as many as 9 million Americans are chronically infected with hepatitis C virus (two to three times the CDC's estimates). The disease can proceed slowly, damaging the liver without the infected individual noticing adverse effects. Infection can lead to cirrhosis (scarring) of the liver and in some cases, liver cancer. The majority of liver transplants in the United States occur because of hepatitis C. Because blood banks did not use a reliable blood test for hepatitis C until 1992, blood transfusions were a leading mode of transmission before that time. Now, accidents involving contaminated needles and hospital workers  and sharing of needles by recreational drug users cause most new cases.
and sharing of needles by recreational drug users cause most new cases.

In this issue
From the CEO / LettersHow Nellie got her groove back
Trapping the mutant virus
Doing a 360 in the WLA
Moving forward
Noteworthy
On Point:
Not the same old, same old
 By Quinn Eastman
By Quinn Eastman
Jim, a technology executive from North Carolina, probably was infected with hepatitis C virus (HCV) through a blood transfusion in the 1970s. But he only found out he had it this spring when his new doctor followed up blood tests showing elevated liver enzyme readings.
Now, the worst part is the uncertainty. "I have a disease that can kill me, but my doctor doesn't advise getting treatment," he says. His HCV is the most common and hardest to treat, so statistically he faces less than even odds of success. And he worries that the side effects of the antiviral treatment - as another patient put it, a "nasty way of getting well" - would impair his ability to work.
It's expensive too. Antiviral therapy costs over $20,000 per year, is effective only half the time against the most common form of the virus, and produces such severe side effects that one in eight patients must withdraw prematurely. Treatment consists of weekly injections of interferon, which ramps up the body's own immune response against the virus, and ribavirin, which may slow viral replication. Rashes, loss of appetite, and flu-like symptoms are the most common side effects, says pharmacy specialist Sybelle Blakey, who works with many hepatitis C patients at the Atlanta Veterans Affairs Medical Center and monitors them closely for psychiatric problems or problems with white blood cells.
While treatment options have improved for people with HCV in recent years, there's still a long way to go. Because the virus comes in many varieties and changes quickly, there are no globally effective vaccines, says Emory gastroenterologist Curt Hagedorn, who wants to attack the disease from a completely different angle. He and other scientists want to anticipate how HCV will mutate in response to drugs and design a trap so that the virus can't escape.
"There are no drugs that directly attack the virus. We don't even really know how ribavirin works," says Hagedorn, who with backing from the NIH and the Cardile Foundation is looking for better medicines to treat HCV. He and his colleagues are looking for clues that will help them predict who will respond to the current treatment and who won't.
In collaboration with biophysicists at the Centre National de la Recherche Scientifique (CNRS) in France and BioCryst Pharmaceuticals in Birmingham, Hagedorn is searching for compounds that inhibit replication of HCV and that could make the current antiviral treatment shorter and more reliable. John LaVoy, an enzyme purification expert in Hagedorn's laboratory, works with CNRS scientists to study hepatitis C polymerase -- an essential part of the viral replication machinery that uses RNA as a template to make the cores of new viruses.
"You can bet that hepatitis C will respond to drugs in the same way as HIV, and that's to mutate like crazy. I think we can build a stronger barrier against that," says Hagedorn. His laboratory supplies the French scientists with purified protein and contributes detailed knowledge about how changes in the polymerase affect its activity.
Finding the right compounds to use as drugs against hepatitis C is where BioCryst enters the picture. In July, the National Institute of Allergy and Infectious Diseases (NIAID) awarded BioCryst, in collaboration with CNRS and Emory, a $600,000 two-year small business grant to test a wide variety of compounds for their ability to inhibit the HCV polymerase in chemical and cell-based assays. They've already identified promising compounds that may jam the replication machinery inside the viral polymerase.
Any new medicine would probably be combined with the current antiviral treatment to bolster it.
That leaves people like Rhonda, a nurse at the VA, keeping her fingers crossed. She's nine weeks into her anti-hepatitis C treatment. "I anticipated terrible side effects, but I haven't had more than a significant headache after each injection," she says. She'll know more soon; the current protocol calls for a halt after 12 weeks if there hasn't been a sufficient drop in virus levels.
Hagedorn, who monitors Rhonda's progress, says too little is known about why some patients respond and others don't. In some cases, the virus comes back after the treatment is finished. Some scientists are looking for signals that could give doctors a hint ahead of time.
Yuri Choi, a postdoctoral fellow in Hagedorn's laboratory, is looking for genes whose activity could explain who responds to the antiviral treatment and who doesn't. She uses a microarray chip about the size of a child's smallest fingernail. The chip is stuffed with probes that allow Choi to examine a tissue sample and determine which genes are turned on and off.
The samples come from liver transplants performed at Emory by surgeon Tom Heffron. Choi has compared the genes turned on from livers with and without hepatitis C virus and, as an extra check, livers from alcoholic patients, who have livers damaged by another mechanism. "It's a relatively new technology, and you get a large amount of data. We have to figure out ways to filter out the noise," she says. She found a few genes that differ between the hepatitis C and alcoholic livers. Scientists have already found that in other situations, some of those genes are regulated by interferon. Other laboratories have used a chimpanzee model of hepatitis C to study affected genes, "but that's misleading because the chimps don't respond in the same way humans do," says Hagedorn.
Eventually, she and Hagedorn will examine patients' biopsy samples to see if the genes pinpointed by scientists so far have been activated and then compare those data with the patients' ability to fight the virus.
Quinn Eastman was a summer science writing intern at Emory.
Copyright © Emory University, 2003. All Rights Reserved.
Send comments to the Editors.
Web version by Jaime Henriquez.