


|
 |
 |
|
|
 |
 t’s
not the way his father learned surgery, at least the first time
around, but resident David McClusky III (left) believes his experiences
in Emory’s virtual surgical environment made him better,
and certainly more comfortable, when he finally operated on a
real patient. “Because I already knew what I needed to be
doing with my hands, and how it looked and felt to do the procedures,
I was able to concentrate more on the patient, rather than strictly
on whether I was doing something right,” he says. t’s
not the way his father learned surgery, at least the first time
around, but resident David McClusky III (left) believes his experiences
in Emory’s virtual surgical environment made him better,
and certainly more comfortable, when he finally operated on a
real patient. “Because I already knew what I needed to be
doing with my hands, and how it looked and felt to do the procedures,
I was able to concentrate more on the patient, rather than strictly
on whether I was doing something right,” he says.
McClusky’s dad, a general
surgeon in Twin Falls, Idaho, was an early adopter of the minimally
invasive surgery (MIS) that is driving surgical training. Patients
and payers alike have embraced new procedures that reduce pain,
scarring, and hospital stays, but for surgeons such as the elder
McClusky, MIS turned what they knew upside down.
“Yes, it took Dad a little
longer to learn than me,” says the son, “precisely
because he was already such an experienced surgeon.”
In MIS procedures, a thumb-sized,
high-resolution video camera and long, narrow surgical instruments
are inserted and manipulated through small “keyhole”
incisions. Surgeons must mentally translate two-dimensional tissue
images on a video screen to three-dimensional images seen in an
actual surgical field. They then must overcome the fulcrum effect,
the visual-sensory mismatch caused when the hand moves down but
the instrument on the screen moves up. Furthermore, the powerful
tactile feedback of direct hand contact with tissue is replaced
by weaker feedback from the instruments, which are attached to
18-inch levers.
“Surgeons used to have to
learn from other surgeon’s mistakes,” says McClusky.
“Now you can learn from your own.” |
 |
| |
|
|
 |

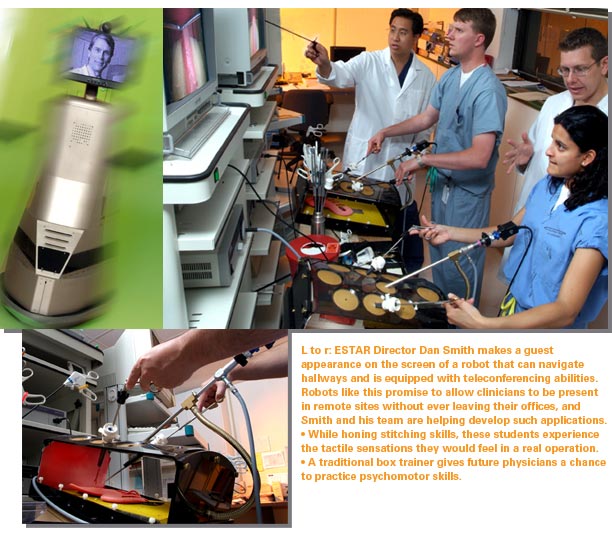
Minimally
invasive surgery is only a part of the revolution that began in
the 1990s, says Emory surgeon Dan Smith, director of the Emory
Simulation, Training and Robotics (ESTAR) program. More and more
procedures are being done laparoscopically, endoscopically, or
via surgical robotic systems, the newest advance. Surgeons use
these remote-controlled devices, connected to computers, to operate
through the tiniest of incisions while monitoring and adjusting
their instruments to account for heartbeat, breathing, and other
physiologic movements.
When used safely, Smith says, these
systems deliver “equalizing technologies” for better
and safer care of patients, extending the range of difficult procedures
that skilled surgeons can perform with less risk and greater comfort
for the patient. However, the new technology and procedures aren’t
intuitive, he says. They “challenge the way human beings
naturally interact with the physical world and thus have enormous
implications for the practitioner and patient, especially for
the practitioners’ first few patients undergoing a new procedure.”
Emory established ESTAR in 2001,
in part because the tools of surgery had changed so radically
in recent years. But other factors came into play as well. Two
years earlier, the Institute of Medicine published “To Err
Is Human: Building a Safer Health System,” highlighting
the issue of medical and surgical errors and ways to circumvent
them using lessons learned in other professions. More recently,
residency training time was reduced to 80 hours per week under
new federal guidelines, necessitating increased efficiency. And
Emory’s medical school is now in midst of a curriculum redesign,
with ESTAR as a key component.
The program designs curricula for
surgical training using the newest MIS technologies. Now increasingly
used by Emory’s own students, residents, and faculty, the
learning modules have wide applicability to other institutions
as well. ESTAR now offers six to 10 continuing education programs
annually, with more on the way, and clinicians and educators from
other institutions arrive regularly on campus to learn how to
add virtual reality, simulation, and robotics to their training
programs. Dissemination of this knowledge is likely to increase
in importance as the American College of Surgeons and the American
Board of Surgery undertake development of new national training
standards.
ESTAR enhances rather than replaces
current methods of education and training, says Smith, citing
cholecystectomy as an example. Young surgeons still get their
information on anatomy and physiology of the gallbladder in traditional
ways. They still learn traditional open-incision cholecystectomy—necessary
in clinical situations like inflammation and bleeding—by
taking incremental responsibility in real-life procedures. However,
more and more, they are acquiring and honing their basic skills,
beginning with suturing, in the simulation lab. When it comes
to laparoscopic procedures, they increasingly turn to the ESTAR
lab. There they progress through a carefully sequenced series
of experiences, learning to move spheres and cubes, manipulating
clips on duct-like tubes, and, finally, performing the entire
operation on a haptic simulator. This simulator includes both
a video monitor and actual tactile feedback as the trainee cuts
away the virtual gallbladder, manipulates it into a little sack,
and withdraws it through the small incision. |
 |
 |
| |
|
|
 |

That’s
what Smith wants to find out. The ESTAR program conducts research
on how surgeons learn and on the effectiveness of the new training
tools. Numerous studies have shown that training on a simulator
makes surgeons better at operating simulators. ESTAR researchers
measure which simulators reduce the learning curve and improve
skills in the operating room and how. For example, urologist Kenneth
Ogan is now teaching 12 Emory urology residents to use an aptly
named “uro-mentor” to treat kidney stones and tumors
in a minimally invasive fashion. In the study, residents will
either train on the uro-mentor or learn skills through traditional
means. Following training, the residents will be assessed on actual
cases in the operating room. The hope is that this virtual reality
simulator will provide residents with necessary skills prior to
entering the operating room, which will result in fewer errors
and improved patient safety.
Smith considers ESTAR a “simulation
and robotics playground.” General and subspecialty surgeons,
interventional radiologists, anesthesiologists, emergency medicine
physicians, and nursing faculty all turn to the program for help
in designing training modules specific to their own needs. Now
tucked away in an Emory University Hospital annex, the playground
will get new digs when a new medical school building opens, complete
with a large simulation laboratory where students can operate
and recreate other patient situations using actors and electronic
models. |
 |
| |
|
|
 |

Current
guidelines for deciding when a surgeon is adequately trained now
depend on his or her completion of a certain number of procedures,
a one-size-fits-all approach. Simulation provides a more precise,
individualized, step-by-step assessment of proficiency, and many
predict readiness will eventually be measured this way. How many
times does a surgeon need to remove an electronic gallbladder
before being ready to operate on a real patient? As many as it
takes, says Smith, just as novice or experienced pilots learning
to maneuver a new plane may crash and burn over and over before
they leave the simulator for the real cockpit. The flight simulation
analogy is used frequently in discussions of simulation training
for clinicians, and for good reason. A decade ago, Smith was present
at the birth of simulation training in surgery––or
at least its adoption from the airline industry. He was part of
the team of physicians, engineers, and behavioral scientists who
studied flight simulators for pilots, and then developed one of
the first simulators for laparoscopic surgery.
The combination of simulators, the
Internet, and robotics has enormous potential to provide remote
proctoring, assessment, and surgical support anywhere in the world,
says Smith. He is discussing such possibilities with medical centers
in Shanghai and Beijing. But first he wants to spend time, robotically
that is, in Idaho. In July, several Emory surgical residents began
a rotation in the elder McClusky’s Twin Falls community
hospital. While the residents operated alongside community surgeons,
Emory surgical faculty monitored their work, able to see what
was happening as precisely and at the same instant as did the
surgeons in the operating room. They then remotely offered critiques
and suggestions. After fine-tuning this pilot, Smith hopes to
incorporate it into continuing education programs, robotically
going home with doctors while they continue to practice and then
perform their first real procedures.
Young David McClusky, like his father,
will welcome them there in the OR. “Everyone has to learn,”
he says, “but some things you simply don’t want to
have to learn first on your patients.”
And for that he can thank the robots.
|
 |
| |
|
|
 |
Sylvia
Wrobel, former associate vice president of Health Sciences Communications
at Emory, writes about science and medicine. |
 |
| |
|
|
|
|
|