|




|
 |
| |
|
|
 |
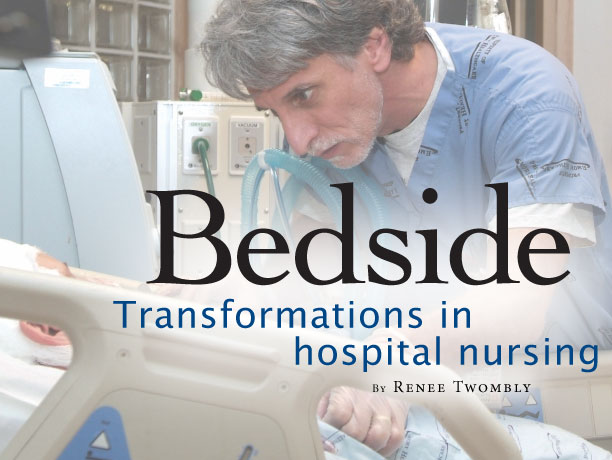
While
having families in the neuro ICU improves patient outcomes, it presents
additional challenges for delivering care for nurses like John Scala,
who has worked in neurocritical care for seven years. |
 |
| |
|
|
| |
 E-mail
to a Friend
E-mail
to a Friend  Printer Friendly
Printer Friendly |
|
| |
|
|
 |
It
was not the same woman that Jason Forche saw lying in the bed in
room 52. One moment Sally R.* was alert and talking. She knew her
name and that she was in Emory University Hospital. A 39-year-old
mother of two, Sally was glad her husband was with her.
The
next moment—just 30 seconds later—Forche, the nurse
responsible for Sally’s care, knew something dramatic had
happened. None of the vividly colored monitors surrounding the bed
had blinked, changed their readouts, or uttered a peep. Everything
seemed the same except Sally had stopped talking to her husband.
To the untrained eye, that would mean
little, but in a neurointensive care unit that treats brain injuries,
nurses are keenly aware of any sign that suggests something is amiss.
Quickly, Forche called the nurse practitioner
in the unit, explained what he had checked and what he thought had
happened, and together they rushed Sally to the diagnostic CT machine
down the hall. The scan was negative. Forche then whisked her downstairs
for an angiogram, and as he feared, Sally was experiencing a cerebral
vasospasm, a potentially lethal constriction of a brain artery.
It had clenched shut, depriving parts of her brain of blood and
oxygen. A quick infusion of strong drugs reopened the vessel.
Sally was back. |
 |
| |
|
|
| |
*
Her name has been changed to protect her privacy |
|
| |
|
|
 |
| |
|
|
 |
Welcome
to 2D ICU, a unit unlike any others at Emory,
or like few in the United States. In both form and function, it
is a place where physicians, nurses, and staff are applying an emerging
model of hospital care.
Here families stay with patients 24/7,
if they like, and clinical care is led by neuro intensivists, a
relatively new breed of MDs who specialize in treating critically
ill patients with brain injuries.
And it is on 2D ICU that nurses are
migrating from the monolithic central nursing station found on most
modern hospital floors back to patient rooms, to be as close to
the bedside as possible—the place where nursing care is traditionally
valued.
Accompanying this transition, these
nurses also are assuming bigger responsibilities. They are providing
input into how patients should be managed as well as what should
occur in a crisis. They are drawing on the newest technology to
provide smoother, coordinated care. They are encouraged to move
up the professional ladder and earn additional certification—and
many do. And in an even bigger way than in the past, they are proving
an indispensable resource not only to patients and their families
but also to the entire clinical team.
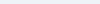
“Nurses are more than my eyes
and ears. They are my eyes, ears, mouth, hands, everything,”
says Owen Samuels, medical director of the neuroscience ICU program.
|
 |
| |
|
|
 |
| |
|
|
 |
Convergence
of forces
The building of 2D ICU represents a convergence of medical, cultural,
and market forces at play in health care, changes that help explain
transformations in hospital nursing.
Foremost among them is that some hospitals
are morphing into a collection of critical care units that treat
the sickest of the sick. Emory Hospital, because of its tertiary-care
status and the breadth of specialties operating here, has long been
one of those facilities with a burgeoning critical care census.
At the same time, because of new national
restrictions on the number of hours that residents and interns can
work, there are fewer residents on the units to treat patients than
before. The traditional resident-fellow-attending academic model
has become strained, and nursing shortages and a dearth of critical
care specialists have plagued hospitals not only in the Emory system
but also across the country.
Simultaneously, health care consumers
have become savvier, more willing to choose a hospital based on
rankings in popular surveys, and on other criteria more akin to
a shopping mall experience—the look and feel of the place,
the customer service.
Even as the Emory neuro ICU was dealing
with these changes, it was growing fast. From a single seven-bed
unit in 1998, Emory’s neurocritical care has expanded now
to include almost five times as many beds in three units. Occupancy
now averages more than 90%, says Ray Quintero, department director
of 2D ICU.
One of the reasons for the rapid development
of the service is that patients are surviving catastrophic brain
injuries thanks to quicker, more advanced treatment. Another is
that many patients are referred here for procedures that are unavailable
elsewhere.
For example, Emory is one of the few
hospitals in the Southeast to offer a less invasive treatment for
aneurysms, or life-threatening bulges in brain blood vessels. This
technique involves threading a catheter through the patient’s
groin up into the brain, and depositing a tiny coil in the bulge
to block blood from entering. More typical treatment for an aneurysm
involves use of a titanium clip to bind the bulge, which first requires
a craniotomy to remove part of the skull.
While placement of the coil is less
invasive, it requires a huge amount of technology in the care of
these patients. And because complications may arise one or two weeks
after coiling or clipping, such treatments require one of the longest
hospital stays of any disorders, Quintero says. |
 |
| |
|
|
 |
| |
|
|
 |
When
nurses practice
Long before 2D ICU was built, Samuels saw how these long stays combined
with resident shortages could damage the quality of care delivered
in the ICU. He turned to mid-level caregivers, what are known as
physician extenders, to fill the “care gap.” These physician
extenders include physician assistants, surgical assistants, nurse
anesthetists, and nurse practitioners (NPs).
NPs are registered nurses who have
completed advanced education and rigorous training in the diagnosis
and management of illnesses. As such, they are able to provide a
broad range of health care services.
On the neuro ICU, “they do all
sorts of complex, high-risk procedures, which would have been unheard
of years before,” Samuels says. Among them are placement of
invasive centralized arterial lines and pulmonary artery catheters
as well as lumbar punctures and drains.
Since NPs stay in the units during
day shifts (with plans to expand coverage to 24/7), they work hand
in glove with physicians, the care team, and, of course, bedside
nurses. The partnership between NPs and bedside nurses is important,
says NP Michelle Ossmann. “Bedside nursing is key,”
she says. “The nurses determine everything, including when
we take action. I can’t function without them.”
As NPs increasingly were given authority
in neurocritical care and as the number of beds and the services
grew, responsibilities also grew for experienced bedside nurses.
With patient safety as the top priority, they have the power to
stop care if they feel uncertain about a process.
“We are more empowered to make
a change,” says Angela Drummond, who has worked in the unit
since 1999. “I question, I ask, I reason.”
Yet through all this increased responsibility
and empowerment, the element that can’t be diminished happens
at the bedside. It is the human touch. |
 |
| |
|
|
 |
| |
|
|
 |
Families
in shock
The tragedy that unfolds daily in the neuro ICU underscores the
fact that anyone can suffer a sudden and devastating neurologic
event. The disorders treated here are not the exclusive province
of the elderly.
“A man can say goodbye to his
family in the morning and unexpectedly be in our unit in the evening,”
says John Scala, who has worked in neurocritical care for seven
years. “Families are often in shock and grief because of the
abruptness of this illness.”
His point was made when, as the night
nurse in charge, he rounded on patients in 2D ICU. On this typical
evening, the patient mix included a woman in her 30s with a cranial
bleed caused by taking ten tablets of ephedra a day to lose weight;
a 31-year-old man in a coma from a steroid-induced stroke; and seven
patients, aged 39 to 72, recovering from aneurysm treatment.
In older models for delivering intensive
care, families in shock huddled together outside the intensive care
unit and were asked to refrain from intruding when the medical team
held rounds to discuss patient care and prognosis. The scenario
was less than ideal, says Samuels.
“Medicine and nursing have become
so complex and so demanding that it has taken both nurses and doctors
farther and farther from the patient’s bedside, both physically
and metaphorically,” says Samuels. “There is less hand-holding,
less hands-on touching, healing, and bonding with patients.”
When Emory administrators decided
in 2005 to expand the busy neuro ICU, Samuels put together a team
of nurses, neurologists, pharmacists, social workers, design experts,
and family members of former patients to figure out how to move
caregivers back to the bedside.
“I think it’s a mistake
to view families as yet another sort of checklist for the doctors
and the nurses to take care of,” Samuels says. “Medicine
in general has neglected the powerful and important role that families
and patients can play in the healing process.”
So the team set about to design a
unit “where the family and the patient are not objects of
treatment but are full participants in the whole healing process,”
he says. And that meant that nurses and families, too, returned
to the bedside. |
 |
| |
|
|
 |
| |
|
|
 |
| |
|
|
 |
 |
 |
| |
|
|
 |
Like
mother, like daughter
In June Sharkey’s experience, the nursing profession
is “completely different now” from when she first
stood by a patient’s bed in a small Mississippi hospital
in 1979. “If a doctor came into the room and you were
sitting down, you got up and gave him the chair,” she
says. “Nurses were no more than handmaidens to the doctors.”
It wasn’t much better
at Emory when she came in 1980 to work on a seven-bed special
care unit for neurology patients and a few overflow heart
patients. Nurses had little say in how the unit was operated
or patients were managed. “It was more like a dictatorship
than a democracy,” says Sharkey (above,
right). “The staff nurses did what the ranks above them
told them to do.”
Yet in 2006 when June’s
22-year-old daughter, April Sharkey (above,
left), joined Emory as a nurse in the same unit as her mother,
she entered a dramatically different environment. The younger
Sharkey’s experience of nursing is as “the patient’s
advocate,” she says.
The change in scenario began
to unfold about 10 years ago for nurses in the neuro ICU when
they first were invited to attend leadership meetings. There,
nurses have come into their own in a way that is still atypical
in other hospitals, both Sharkeys say. For example, June Sharkey
now can do such things as manage drug titration if a patient’s
status changes. “Our autonomy has increased,”
she says. “The majority of doctors here are open to
my input.”
In this new climate, nurses
also are pushed to do more, she says. “The patients
are sicker, and there is more technology to help us monitor
them. We have many more responsibilities in addition to the
typical bedside duties.”
April Sharkey, who received
her nursing degree from Emory less than two months before
she started working in 2D ICU, finds neurology to be a challenging
area for nursing. “You have to keep up with the research,”
she says. “I can’t believe how much I learn every
day, and after a 12-hour shift, I feel I have made a difference
in someone’s life.” |
 |
| |
|
|
|
 |
| |
|
|
 |
Fine-tuning
form
There is no other critical care unit like 2D ICU in Atlanta, and
few in the country. Its form has helped further define the function
of the patient care team.
Patient-centered care is not new in
Emory Hospitals. The hospital care teams have followed the philosophy
for years, but they have been hampered by the design of the physical
plant. By contrast, 2D ICU, which opened in February, features a
new design tailored for 21st-century health care. Among its features
are a large waiting area for family members, with a kitchenette
and a children’s play area on one side. Like a hotel concierge,
two assistants take turns staffing a welcome desk, offering solace
along with towels for the shower room or soap for the washer and
dryer. Within each patient room is a separate studio area for family
members, with chairs that open into beds. Soon, the suites will
have laptop computers.
When not at the bedside or in treatment
areas, nurses work from alcoves situated between patient rooms.
They have only to glance in to see and hear the patients and to
monitor IV fluids and a myriad of machines. Often, a probe is embedded
into the brain to measure temperature, oxygen, and intracranial pressure, and transcranial Doppler ultrasound is
available to look at the velocity of blood flow. A CT scanner is
just steps away.
and intracranial pressure, and transcranial Doppler ultrasound is
available to look at the velocity of blood flow. A CT scanner is
just steps away.
Families come and go and are welcome
to talk with physicians and nurses during rounds. Their presence
has put nurses front and center to answer questions and provide
information. Quintero sees this change as positive, emphasizing
the needs of the patient before those of the medical team.
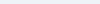
To create an environment where nurses
become invested and can contribute the most, Quintero has turned
to the nurses themselves. “I tell them, it’s not my
unit. It’s your unit.” Creation of 2D ICU involved shared
decision-making, a process that sent a team of nurses across the
country to search for the perfect equipment boom for the patient
rooms, among other tasks.
“I was amazed that I was asked
to go,” says June Sharkey, who has worked as a nurse for 27
years. “They listened to what I had to say about one of the
most costly decisions to be made in the unit.”
“I know what nurses need because
I am a clinical nurse too,” says Quintero, who has 25 years
of hands-on nursing experience, including 20 years as military nurse
in Texas at the Air Force’s largest hospital.
However, changes in the environment
may have unknown consequences for nurses, says John Scala. “Until
you build it and live in it, you don’t know how it works,”
he says. “We work at a high stress level anyway, but now we
have to explain everything we are doing to everyone and act as both
educator and psychologist. The thing that makes it okay is that
we all know it is the right thing to do.”
The adjustment can take some time.
“It was difficult at first,” says Angel Sostre, a nurse
and the day shift clinical manager. Recently Sostre came from a
trauma ICU in Miami, where he learned to work fast and on his own.
“Having family around when I want to do procedures took an
adjustment on my part. I felt I was crowding them,” he says.
“But once they build a trust in me, the family will let me
do my job. It works as long as we understand the roles each of us
plays.”
Everyone in 2D ICU is adjusting, figuring
out what works and what doesn’t, and where the limit exists
for just how much nurses can do, says Samuels.
“In trying to establish a new
standard for providing care for these critically ill patients and
their families, we are all pushing the envelope,” Samuels
says. “Creating this new culture doesn’t have a beginning
and an end: it’s a process, and it’s an extremely challenging
one at that.” |
 |
| |
|
|
 |
| |
|
|
 |
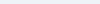
Taking
it to the next level
In a sense, 2D ICU is a demonstration unit that is transforming
the culture of patient care, says Susan Grant, chief nursing officer
for Emory Healthcare. The lessons learned here will help shape the
form that future intensive care units in the proposed new Emory
Hospital complex will take.
“Having family members in a
unit 24/7 changes clinical practices, challenging the old way of
doing things,” says Grant. “It is not a small thing.”
But just as family-centered health
care, along with new technology and better designed physical space,
improves outcomes, so does the evolution of nursing practice.
Grant herself began her professional
career as a bedside nurse at Emory. In the 20 years since, as a
nurse and nursing administrator serving in educational institutions
across the United States, she has witnessed firsthand the changing
profession. “We are far beyond Florence Nightingale’s
day, for sure, but we have gone miles beyond what nursing was even
five years ago,” she says. The professional practice of nursing
now is responding to and being proactive around technology, research,
medical advancement, reimbursements, regulations, risk aversion,
and disease management, Grant says. Nursing as a discipline needs
especially to be more central to the health care administrative
process.
For all those reasons, Grant is taking
nurses throughout Emory Healthcare on the kind of progressive journey
that neurocritical care has navigated. She is seeking to have the
entire Emory Healthcare system awarded “magnet” recognition,
bestowed by the American Nurses Credentialing Center. Magnet status
is exceedingly hard to come by. Only 11 health care systems have
been so designated since the program began more than 20 years ago.
Only 4% of U.S. hospitals—238 out of 5,764—have earned
these credentials, which may take up to seven years.
The magnet program is designed to
provide consumers with the ultimate benchmark by which to measure
the quality of care offered by nurses, and by extension, their institution.
“This is not window dressing. High nursing standards really
improve patient care,” says Grant, who in a previous position
led the University of Washington Medical Center through two renewals
of credentialing for the magnet program.
“In many ways, issues of patient
safety have really forced this movement,” Grant says. “To
address them, health care is learning a lot from aviation and other
high-risk industries. To ensure safe flight, everyone on the flight
team—not just the pilot—has to be able to say something
is not right when it deviates from the routine standard of care.”
Emory Healthcare has already instituted
a “shared decision making” structure across its system
to include input from workers at all levels as well as from families.
And on the floors, nurses are engaged in “unit practice councils”
that identify practices that could be improved and then determine
how to make that happen.
Angela Drummond leads the effort in
the neuro ICU. The 13-member council has identified bloodstream
infections and
ventilator-associated pneumonia as two areas of concern. Nurses
have researched the existing rates, matched these to national averages—“too
high,” Drummond says—and are now seeking ways to lower
the incidence. In the space of just two meetings, they have found
that two very low-cost yet high impact solutions will help:
proper hand-washing on the part of all clinical staff and mouth
care for patients every four hours.
“This encourages nurses to practice
evidence-based nursing, and we are all excited about it,”
Drummond says. “We are working hard to get the number of those
infections down, which will improve outcomes.”
Magnet designation also comes when
nurses develop professionally, and on that score, Emory has a good
leg to stand on, says Grant, who also serves as the first assistant
dean for clinical leadership at the Nell Hodgson Woodruff School
of Nursing.
“As far as nursing education
goes, you can do anything at Emory Healthcare,” Drummond says.
The neurocritical care nurses seem
to take that slogan to heart. Of the 87 registered nurses working
in the three ICUs, nine are taking graduate courses, and six are
studying to be nurse practitioners.
Ironically, a commitment to staff
advancement also has the potential to create rapid turnover in nurses
and even shortages—the very thing professional development
is supposed to bring to an end, says Sharkey, who spends a lot of
her time training new nurses.
Part of the challenge on this frontier
of transforming health and healing, then, is to balance new empowerment
and knowledge for nurses with the traditional hands-on care they
deliver at the bedside. That will create the strongest kind of magnet
for patients and nurses alike.
“This is a more humanized kind
of health care,” Drummond says. “The feeling now is
that we are all in this together.”
Videos
about the neuro ICU
Renee
Twombly is a freelancer who writes frequently on health care topics. |
 |
| |
|
|
| |
|
|
|
|
|

