Printer friendly E-mail
a friend

Dean Thomas
J. Lawley
| Class of 2011 | ||
| 133 students: 67 women, 66 men Age Range: 20 - 35 years old Mean Undergrad GPA: 3.70 Mean MCAT: 34.4 Students with Postgraduate Degrees: 11 |
||
| Curriculum Steering Committee | ||
| Andrew Adams Wayne Alexander Sarah Berga Jo Ann Dalton Joel Felner Justin Golub Steven Gorbatkin Kate Heilpern Thomas Lancaster Richard Levinson Fadlo Khuri Joseph Kinkade William McDonald Larry McIntire Richard Nichols Alan Otsuki Tristram Parslow Jessica Risser Ira Schwartz Barry Shur Robert Smith III Joanne Williams Vincent Yang James Zaidan Executive Committee |
||
A Watershed Year
Adapted
from the Dean's State of the School Address,
October 9, 2007
It’s been a watershed year in many respects. We have a new curriculum, a new medical education building, a commitment of new education resources, new department leaders, new achievements in research and clinical care, and so much more.
Education is the mission that defines the School of Medicine because while not all of us are researchers or clinicians, we are all educators. We now have 480 medical students. The entering class, the class of 2011 is made up of 67 women and 66 men, who were chosen from more than 6,000 applicants. These students came from a variety of undergraduate institutions. Emory contributed the most to this class—22 this year—while we had eight from Harvard, six from Cornell and Georgia, and five from Duke, among other schools. In addition to biology, biomedical engineering, and chemistry, these students majored in creative writing, Hispanic studies, Italian, German, Russian, Spanish, and visual arts. This is a diverse, intellectually rich group of individuals. Their mean undergrad GPA was 3.7, and their M-CAT score, 34.4, ranks them in the 94th percentile.
When the Class of 2011 and others graduate, it’s very important to us that they choose their specialties based on their interest and skills—not on future income, for fear of financial hardship created by student debt. So we’ve been working hard to increase scholarship money available for students. We held steady at about $4 to $4.5 million from 2002 to 2006, but a number of medical school faculty and administrators and development staff have been out on the road, meeting with alumni and friends of the school to raise money, and we now have $6.9 million available for scholarships this year.
The class of 2011 is the first to experience our new curriculum. I can remember standing here three years ago and announcing my intention to create a new curriculum and complement it with a new medical education building. That seems like yesterday. The curriculum steering committee was responsible in large part for putting it together, and I want to thank all of them—students, administrators, and faculty from the School of Medicine but also from the School of Nursing, Emory College, and the School of Public Health. The members of the executive committee deserve special commendation, particularly Jack Shulman, Art Kellermann, Steve Warren, Carlos del Rio, and Bill Eley.
The first 18 months of our curriculum is structured so the first months focus on the “healthy human” and the subsequent 12-14 months on human disease. Students and faculty are invigorated and working more closely than ever before. Faculty have been exceptional in both planning and delivering the curriculum. The students, we understand, actually are attending class. How about that? Seven patients have been presented so far to the students, and amid all the lectures and group learning that they’ve been undergoing, they’ve had their initial training in taking a history and conducting physical exams.
We start students out with a week on the wards—their last view of medical care as a layperson. The prologue—the so-called big picture—is taught with input from anthropology, the School of Public Health, and the School of Nursing, as well as the CDC. Faculty participation rose to new heights when Dr. Gordon Churchward showed his own stress test while riding an exercise bike in front of the class. All in all, it’s been an excellent start.
We listened carefully to our students, as well as our educators, and designed what I think is the finest medical education building in the country. We created a student-friendly building with spaces where faculty and students can interact outside the classroom. But the building is also a place for grand rounds, seminars, social events, and classes. We want faculty to use it and to use it often and come in contact with students outside the classroom. The building has a state-of-the-art teaching space, including lecture halls, computer rooms, 20 small group classrooms, 16 OSCE rooms, and 5,000 sq. ft. of simulation space that can be used to model an operating room and emergency room bays.
Now let’s switch gears and look at our research enterprise. We are coming to the end of our second major strategic research plan. We drafted our first one in 1997, and as a result of that plan, we’ve built 400,000 sq. ft. of research space, and we recruited more than 100 funded investigators. In 2002 that plan lapsed, and we then went into our second phase and produced a plan that created yet more research space and focused on multi-investigator grants, large P-series grants, and program projects. We’ve executed our research plans in good days when NIH funding was plentiful and in not so good days when NIH
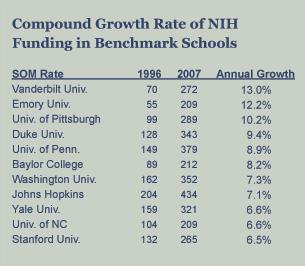 funding is very tight. Regardless, our research program has grown continually. In terms of NIH funding, the SOM is 18th in the nation, with $209 million this year, an increase of 9% over last year. We’ve made terrific progress—in 1996 we were ranked 31st and had $55 million in NIH funding.
funding is very tight. Regardless, our research program has grown continually. In terms of NIH funding, the SOM is 18th in the nation, with $209 million this year, an increase of 9% over last year. We’ve made terrific progress—in 1996 we were ranked 31st and had $55 million in NIH funding.From 1996 to 2007, the average annual compound growth rate for the medical school has been 12.2%. That growth is due to the hard work and ability of our investigators. Securing grants and contracts is an indicator of how well our research strategy has played out. Some of this year’s top grants include $33 million to the Influenza Center of Excellence, a $31 million Clinical and Translational Science Award (CTSA), $25 million to the Emory Children’s Center, and a $12 million Specialized Program of Research Excellence grant to the Winship Cancer Institute. In 1996 we had seven investigators who brought $1 million or more in grants annually. Now we have 64.
Clinical Care
Our clinical enterprise in my opinion is better than ever before, and collaboration among the School of Medicine and Emory Healthcare, Children’s Healthcare of Atlanta, and the Atlanta VA Medical Center, is good and strong. We deliver more care than we ever have before; it’s both more sophisticated and more compassionate than it ever has been before.
I asked each of our health care partners to tell us what they were most proud of during this past academic year.
Emory Healthcare (EHC)—Major accomplishments in 2007 included reformulating a five-year strategic plan. Also important is the establishment of an Emory Healthcare-wide office of quality control, with chief quality officers at each hospital and clinic. EHC also has championed its development of integrated patient and family-centered care, which is steering the design of new patient facilities planned for the future. EHC has completed the initial phase of the new clinic’s master plan and is enjoying a robust operating margin this year.
VA Medical Center—Our relationship with the VA is a national role model for excellence. The VA increased its faculty positions by 28 to a total of 175 and added 10 residency slots, for a total of 125. We’re also breaking ground soon on a new research building jointly funded by the School of Medicine and the VA foundation. Also, in the spirit of building bridges, we will complete the long-awaited Lullwater bridge between our campuses.
Emory Children’s Center—The Emory Children’s Center, which is jointly governed by Emory and Children’s, completed its first year of operations under this co-management, with strong financial results. Children’s completed the transition for the management of Hughes Spalding Hospital at Grady and also played an important role in the development of our CTSA grant. It’s also funding several new pediatric subspecialty fellowships as part of our close collaboration.
| Some facts about Grady | ||
|
||
Grady’s been in the news a lot over the past few months, and those of you who work at Grady are well aware of the details and issues. We have been, and are to this day, outstanding partners of Grady. But Grady owes us a lot of money, and at the end of the day we can’t continue to bear the huge financial burden because the counties and the state haven’t stepped forward. We also must be able to educate our medical students and our residents in appropriate facilities and deliver a high standard of care. If we were to perceive that we could not do that, we would have to seek other venues. I want to salute the physicians and the staff who teach and deliver care at Grady. You do a marvelous job.
I want you to have the facts about the relationship between the School of Medicine and Grady so you can be champions in your communities for Emory and Grady. There are several prevailing myths about Grady. One is that Emory is somehow taking advantage of Grady. Nothing could be further from the truth. We do not make money at Grady. In fact, we lose millions of dollars annually and yet provide high-quality medical care more cost effectively than Grady could provide on the open market.
The second allegation is that Emory is cherry-picking paying patients from Grady. In the past year, only 30 inpatients were transferred to Emory Crawford Long Hospital from Grady. Half of them were uninsured, and the other half were mostly Medicaid. An additional 20 outpatients were sent to Crawford Long for medical services unavailable at Grady and then returned to Grady for the remainder of their medical care. There is no financial incentive for physicians to transfer patients to any Emory facility.
The third concern is that Grady pays unfairly for Emory’s malpractice insurance. The Emory-Grady contract, as well as the Morehouse-Grady contract, calls for Grady to pay for malpractice insurance. Grady agreed to this in part because of the high percentage of uninsured patients treated at Grady whose care is uncompensated.
Finally, the fourth misperception is that a Grady “audit” exposed Emory deficiencies. The Cherry, Bekaert, and Holland (CBH) report was commissioned by the Fulton-DeKalb Hospital Authority and was not an official audit, even though Emory wanted a true audit. The assessment affirmed that Emory and Morehouse were in compliance with the contract, and it showed the School of Medicine provided a greater number of physicians and full-time employees than the numbers for which it has been compensated for many years. It also showed that Emory and Morehouse subsidized Grady by $8 million a year for salaries of residents’ supervisors. It showed Grady was not paying our teaching faculty at the agreed-upon scale. After this report was done, we asked the Huron Consulting Group to come in, and they confirmed that we were following nationally recognized standards for faculty time reporting. The CBH report, though, did recommend that we move to more frequent time reporting, which we have done after developing our own electronic system at our expense.
Now let me briefly touch on four truths. One is that the medical schools are Grady’s biggest bargain. Our residency training programs generate approximately $20 million per year for Grady from federal and state resources to reimburse Emory resident salaries and supervision. The total net cost to Grady for all of Emory’s physicians we provide there is only 3.6% of the hospital’s budget. We, of course, supply 85% of Grady’s medical staff, 300 full-time attending physicians and 377 residents. It would be impossible for Grady to find this kind of medical care on the open market at that price.
The second truth is that the medical schools have been carrying Grady’s debt. Grady is supposed to pay our invoices in 10 days, but they are now up to nine months late. The medical schools are the only contractors who are not paid promptly. Currently, Grady owes Emory and Morehouse more than $63 million, and the medical schools cannot continue to be Grady’s bankers.
The next truth is that Grady is vital to the metro region and to Georgia. Approximately one in four physicians in Georgia have trained at Grady. It’s the only level 1 trauma center between Macon and Chattanooga. Grady is north Georgia’s only safety net for pandemics and mass casualty accidents.
The last truth is that time is very short. Grady could run out of money by the end of this year. We’ve endorsed an audit of Grady’s use of state funds, but if we put everything on hold while that is completed, I’m concerned that it’s going to be too late for Grady. We endorse the Metro Chamber Task Force’s recommendations, which should be adopted as soon as possible.
| Dean's Teaching Excellence Awards 2007 | ||
Lisa Bernstein |
||
| Task Force on Faculty & Staff Development | ||
Faculty Staff Ex Officio |
||
Faculty make Emory School of Medicine what it is. They are the heart and soul of the school, and I truly do appreciate all that they do on behalf of Emory and the SOM.
We’ve completed searches and have appointed five new chairs: Carolyn Meltzer of Radiology, Brian Leyland-Jones of the Winship Cancer Institute, Kate Heilpern of Emergency Medicine, David Burke of Rehabilitation Medicine, and Tim Olsen, who will be the new chair of Ophthalmology January 1. I’d like to acknowledge the individuals who have been the chairs of those departments: Arthur Kellermann began the Department of Emergency Medicine and turned it into a top 10 department. Thomas Aaberg has been chair of Ophthalmology, also a top 10 department, for 20 years. I’d also like to acknowledge Bill Casarella. Bill is really a man for all seasons who’s been acting chair of rehabilitation medicine for the past several years.
Everybody is aware that the SOM has a big faculty, but some of you may not be aware just how big it is. We have 2,072 full-time and part-time faculty. That doesn’t include our volunteer or adjunct faculty, who number about 1,000. Faculty, and sometimes even the chairs, don’t appreciate the volume of faculty actions that are processed in the dean’s office through various committee approvals. This past year, we completed processing 606 faculty actions. We had a banner year for senior appointments and promotions—almost double the usual number. It speaks to the excellence of our faculty and to all of their accomplishments, and I’d like to take time to thank those in the faculty affairs office, which is overseen by Dr. Claudia Adkison, who do such a great job.
Our faculty, both full-time and part-time, are about 2/3 male, about 1/3 female, and 12% minority. However, senior faculty—associate and full professor—are about 80% male and 20% female. New hires of senior faculty from this past school year were 75% men and 25% women, and we continue to work to increase the number of female senior faculty. Last year, I appointed Carlos del Rio and Kate Heilpern to chair a task force on faculty and staff development. The group consisted of people with diverse backgrounds, job descriptions, and viewpoints, and their required reading materials included the SOM faculty survey, a University climate survey that had been done about a year ago, an earlier President’s Commission on the Status of Women survey, and a human resources workforce summary. The charge of this task force was that we want the SOM to be the best place to work in Atlanta and to be the best among U.S. medical schools. We want faculty and staff to make valuable contributions and to know their contributions are appreciated. We want faculty and staff to be included in the vision and goals and accomplishments of the School of Medicine.
The task force came up with many recommendations, and these are the top several, which focus on recognition, mentoring, and leadership: The first is to provide personalized recognition for accomplishments in all departments. Second, facilitate training for chairs and division directors in faculty and staff development, incorporate faculty development and mentoring into chair evaluations, and provide more faculty development courses in leadership and teaching skills. Other recommendations include appointing an assistant dean for staff development, expanding mentoring programs across the school, reviewing SOM promotion and tenure guidelines, and reviewing the possibility of creating a clinician educator track. I’m proud to say we plan to implement every one of these recommendations. We expect to report back in the spring or fall as to the progress we’ve made in these areas.
My state of the school address last year detailed the growing challenges within schools of medicine in conflict of interest. I followed that up by asking Drs. Tristram Parslow and Ned Waller to chair a task force on revising our conflict-of-interest policy. The task force has done a superb job in analyzing conflicts of interest across the nation and then bringing recommendations home to Emory for us to utilize. I wanted the task force to review our individual and School of Medicine relationships particularly with pharmaceutical, device, and equipment companies; to address these relationships in the areas of research, education, clinical practice, and administration; and to make recommendations on guidelines and policies. And they have begun to do so.
First, the task force found that we do a good job on managing conflicts of interest in research, although they suggested some small refinements. The task force also made preliminary recommendations touching on the creation of a culture of sensitivity to conflicts of interest as we carry out our daily interactions. They also want to focus on education and policy in institutional conflicts of interest: decisions on investment or technology transfer where the University has a financial interest; administrative conflicts, or decisions by administrators who have financial conflicts; conflicts in education—the influence of industry on CME, sponsored conferences (food, pens, the usual) that can sometimes occur; and finally, conflicts in clinical practice and in gifting. The task force will be bringing recommendations back to us later in the year.
Next year, the task force will continue to refine recommendations in the draft policy. The members want to hold several educational seminars early in the winter, bringing in outside speakers and inviting wide participation and discussion of draft policy proposals. We hope to get that done in winter and early spring and then finalize policies in ongoing educational programs in the late spring. I can tell you that this is a matter of great importance to me, and I know it is a matter of great importance to schools of medicine throughout the country. We do a good job overall. We can do a much better job, though, and this task force will help point the way for us.
The future is very bright for Emory. Despite the status of the NIH budget and the tension around Grady, I am extremely optimistic about the future of the School of Medicine. We have brilliant, hard-working faculty. We have got an exciting new curriculum and outstanding medical students. We have got a new School of Medicine building that supports the curriculum. We have an outstanding clinical enterprise that is doing well. We hope that approval for a new research building will come this year. A new research strategic plan will soon be in the works.
In my 19 years as a faculty member here and 11 years as dean, I have seen a remarkable transformation in this institution. Excellence in every single one of our missions has increased. New clinical facilities are going to be wonderful for our faculty physicians and patients. Our focus on quality at Emory Healthcare is exactly the right thing to do and is another sign of the excellence that surrounds us. Our new research building will help us advance toward our goal of top 10 status, and the ongoing development of our interdisciplinary centers will stimulate new discovery and strengthen our collaboration with partner institutions. Our global reach is expanding rapidly and providing new horizons for research and educational opportunities. The Health Sciences Center and the School of Medicine’s strategic plans complement each other and together move the whole University forward.
With all of the growth and with the increasing standards and expectations, what has not changed in my 19 years here is the collegiality within the School of Medicine, with other parts of the University, and with our clinical and our research partners in Atlanta and elsewhere. It’s not an accident. When we hire chairs and faculty, we purposely determine not only their intellectual and clinical excellence but also their spirit of collaboration and collegiality. It is a hallmark characteristic that truly sets us apart and gives us a sustained competitive advantage. The School of Medicine used to be mainly noted for its strong clinical programs, but now it’s recognized as a leader in research and education as well. Our contributions to health and science are now recognized around the world. It would be easy for us to lose sight of one of the great strengths that differentiates us from our competitors as we grow—the warmth and the openness, the interdisciplinary collaboration of the faculty. I want us all to continue to foster and nurture it. It’s the basis for our great success, and it makes this a much better place to be and to work.
Now don’t get me wrong, we have a long way to go. Everything that we do can be improved, but we clearly have an opportunity to be a top school and a top academic health center. And while the destination is important, I think the journey is just as important. Being top 10 or top 15 is simply a surrogate for quality and excellence in everything that we do and the joy and pride, I hope, that we take in doing it. Top status is simply a road sign that says we’re on the right highway. The number means that all of us are engaged every day, doing our part and feeling glad and proud to be on the journey right here at the School of Medicine. Let me conclude by saying that it’s been my great pleasure to be part of this journey in this School of Medicine for many years. Thank you very much.
—Thomas J. Lawley, MD